I promised that I would share more about our IVF journey in our Pregnancy Announcement post, so this post will be entirely dedicated to the details of our process!
Note that I am not giving medical advice in this post, I am simply sharing our journey and experience! If you have any medical questions, consult with a medical professional.
We decided to go down the IVF route less out of necessity and more because of our general age. Eric and I are both in our mid-30’s and thought it made the most sense to retrieve and preserve some embryo’s sooner rather than later. We started talking about IVF in early Fall 2020 and made the decision to proceed shortly thereafter. From there, we needed to work out all of the logistics of the process. From administrative things like insurance coverage all the way to the scientific side of things like ovulation timing.
BE PERSISTENT
I won’t sugarcoat it, our overall process was not as smooth as we would have liked. We learned many things the hard way, which caused a lot of stress and despair. Our first nightmare occurred when we solidified our fertility plan and got our first bill. To my utter shock, we received an itemized bill for almost $10k. I immediately burst into tears and felt an overwhelming sense of despair. I called the doctors office and they walked me through what each item was and confirmed that they appeared to not be covered by our insurance. I am not one to just sit back and so I decided to take matters into my own hands. Maybe it’s the lawyer in me, but I couldn’t accept the bill until I knew, beyond a shadow of a doubt, that it was correct.
After spending hours on the phone with the insurance company (make sure you speak with your insurance carrier’s authorization department), I was able to confirm that, in fact, every single item that I was getting charged for out of pocket (other than one tiny thing), was actually fully covered. Eric and I were obviously ecstatic but we were also so annoyed. How could this doctors office be so careless, inattentive and irresponsible that they could ask us to pay thousands of dollars out of pocket for a fertility procedure that was fully covered by our insurance? Our bill immediately went from $10,000 to $600! At that point, we decided that we needed a second opinion because we started to feel like we were being completely taken advantage of.
Over the next month, we met with other doctors and attempted to get our records transferred, which turned out to be a nearly impossible task. What we came to realize is that despite not being 100% happy with the administrative side of our experience, the grass was not necessarily greener on the other side. We found that many of the offices were unorganized and didn’t return calls or messages. In the interest of time and not wanting to go back and get our whole IVF procedure plan re-authorized by our insurance company, we opted to stay with our original doctor and push forward.
What I will say is never leave anything this important up to someone else. Nobody will ever care about you and your needs as much as you and your significant other. If you hear something that doesn’t make sense, don’t be afraid to ask questions and challenge why something is the way they say it is. Get familiar with the secretary’s and nurses at your doctor’s office because they can either be your best friends or your worst nightmares. Also get familiar with your insurance company! Sometimes, the difference between coverage and non-coverage is a simple blood test and without it, you’re paying huge amounts out of pocket. In this scenario….BE PERSISTENT!
I do know that fertility treatments are not covered by everyone’s insurance. This was simply our experience. Either way, I would still suggest checking in detail regarding exactly what is and is not covered. You never know!
STIMULATION
We were originally slated to start stimulation medications around Thanksgiving, but that is where things got dicey. Partially because of COVID, many of the medications that were prescribed were backordered or out of stock. On top of that, because many of these meds are considered specialty prescriptions, they can’t always be filled at your local CVS Pharmacy. Our insurance required us to go through a Specialty Pharmacy that was mail order only. Despite my doctors submitting my prescriptions about a month in advance and me scheduling the delivery, I received a call the Friday before Thanksgiving (only a week before I was supposed to start meds) saying that everything was backordered and they didn’t know when they could fill the prescriptions.
Talk about another nightmare! I spent the next 6 days on the phone with my insurance company, doctors office and the specialty pharmacy trying to get these meds or an authorization to fill the prescriptions elsewhere. Eric and I were hosting Thanksgiving, and our poor families basically watched the drama unfold in real time for those 6 days. I don’t think I’ve ever been more stressed out or felt more hopeless than I did during that time.
Despite speaking with many extremely helpful people on all sides, we simply weren’t able to get the medication we needed in time to start our IVF cycle in November/December. It was truly devastating. I knew that we could just postpone one month and it wouldn’t really mean anything in the grand scheme of things, but having done all I could do for 6 days straight (literally on the phone for hours every single day), it was just a really hard pill to swallow.
My piece of advice here is that if you decide to do IVF, or any fertility treatment that has a tight timeline for that matter, make sure you order and receive all of your meds WELL IN ADVANCE. In the end, postponing a month allowed Eric and I to enjoy Christmas and New Years without the stress of being in the middle of an IVF cycle, so I can look back now and see the benefit, but at the time, it seemed like the end of the world. We ended up starting our stimulation meds on New Year’s Day. Our particular plan required us to inject medication into my upper thigh. We alternated each night to allow for healing time and overall, I didn’t bleed or bruise too much. I personally feel like shooting into the thigh is preferable to the stomach, but it all depends on the type of medications your doctor is prescribing. I was being monitored almost daily with blood tests and follicular sonograms so that the doctor could adjust the medications as necessary. This stage typically takes anywhere between 8-14 days. The first few days included shots that stimulate the ovaries into producing multiple follicles. At a certain point during the stimulation period, my doctor also added a suppressor, which suppressed my body from actually ovulating, therefore allowing the follicles to further “ripen” without being pre-maturely released. I ended up on the stimulation/suppression medications for the full 14 days and then, when the time was right, we were told to administer the “trigger” shot, which is the final stage before a retrieval. The trigger shot let’s your body know that it is ready to ovulate so that the final stage of “ripening” can happen for the follicles that you’ve spent time growing.
During this time, the only discomfort or real symptoms I experienced was bloating. As you stimulate your ovaries, they begin to enlarge and by the final days, it was a bit uncomfortable. I didn’t find that I had any mood swings or other negative reactions to the medications.

RETRIEVAL
Once we administered the “trigger” shot, our retrieval had to take place within 36 hours. I was promptly scheduled for my retrieval the second morning after the shot was administered. In preparation for the retrieval, I had to fast the day of the procedure, as I would be going under anesthesia and begin taking an antibiotic and steroid. Because you are fully put under anesthesia, you have to have someone drive you to and from the procedure. My mom was able to come with me since the procedure was scheduled in the middle of a weekday. The retrieval itself didn’t really scare me, but I have a severe fear of needles, so I was really nervous for the anesthesia. My arms were so beat up after having my blood drawn and monitored in the 2 weeks leading up to the procedure that they actually had to administer my IV through my hand (which was painful…I’m not gonna lie) rather than in one of my arms. The anesthesia stung a bit as it went in, but I quickly felt the effects, which are almost like being drunk, and then about 15 minutes later, I woke up in the recovery room.
The doctor was able to tell me how many eggs were retrieved right on the spot and let me know that they would be fertilizing them that same day. They called me the very next day to confirm how many eggs successfully fertilized and were now growing into embryo’s (the medical term is blastocyst). From there, it was just a waiting game to see how well the embryo’s did in the lab. The embryologist was monitoring their progress, which usually takes 3-5 days to reach a particular stage that is safe for transfer. Some of my friends told me that they received daily updates about their embryo’s, but I didn’t hear anything specific up until the day they called me to schedule my transfer, which was to take place exactly 5 days after my retrieval. During this time, I remained on antibiotics and steroids, which were meant to fight off any potential infection or inflammation caused by the retrieval.
When I got home, I pretty much spent the entire day in bed. I was still a little loopy from the anesthesia and I ended up falling asleep with a heating pad on my stomach for a few hours. I was able to take extra strength Tylenol for the cramping, which definitely helped (but check with you doctor before taking anything). The cramping isn’t terrible, it just feels like severe period cramps. I was able to be up and about the next day and my cramping mostly subsided by the third day.
TRANSFER
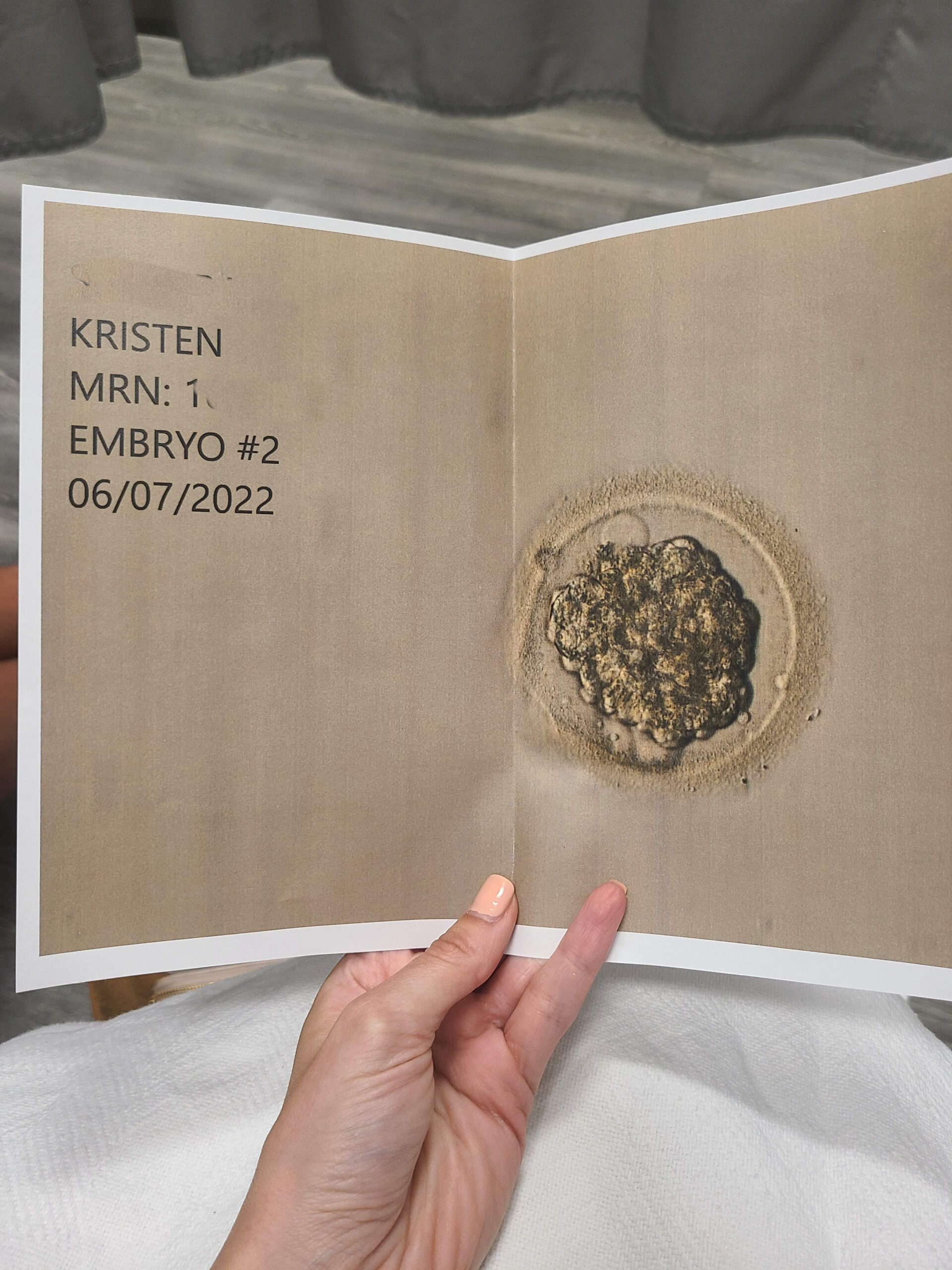
On the day of my transfer, even though I wasn’t being put under anesthesia, the doctor still required that I have a driver to and from the procedure. I was given a mild sedative to reduce anxiety, which I took on my way to the procedure. Before the procedure, my doctor and I spoke about how many embryo’s made it to day five and we discussed how many embryo’s we wanted to transfer vs. cryopreserve (ie. freeze). We decided to only transfer one embryo and freeze the rest. The procedure itself took less than 5 minutes and was virtually painless. The embryologist gave a catheter containing the embryo to the doctor, who inserted the catheter while watching a sonogram screen. After he released the embryo into my uterus, the embryologist confirmed that the embryo wasn’t stuck in the catheter and then I had to lay in the procedure room for about 15 minutes. Eric was able to be there for the procedure via video chat.
After both the retrieval and the transfer, I was told to take it easy and limit any exertion. From there, it was the dreaded two-week-wait (TWW).
TWO WEEK WAIT
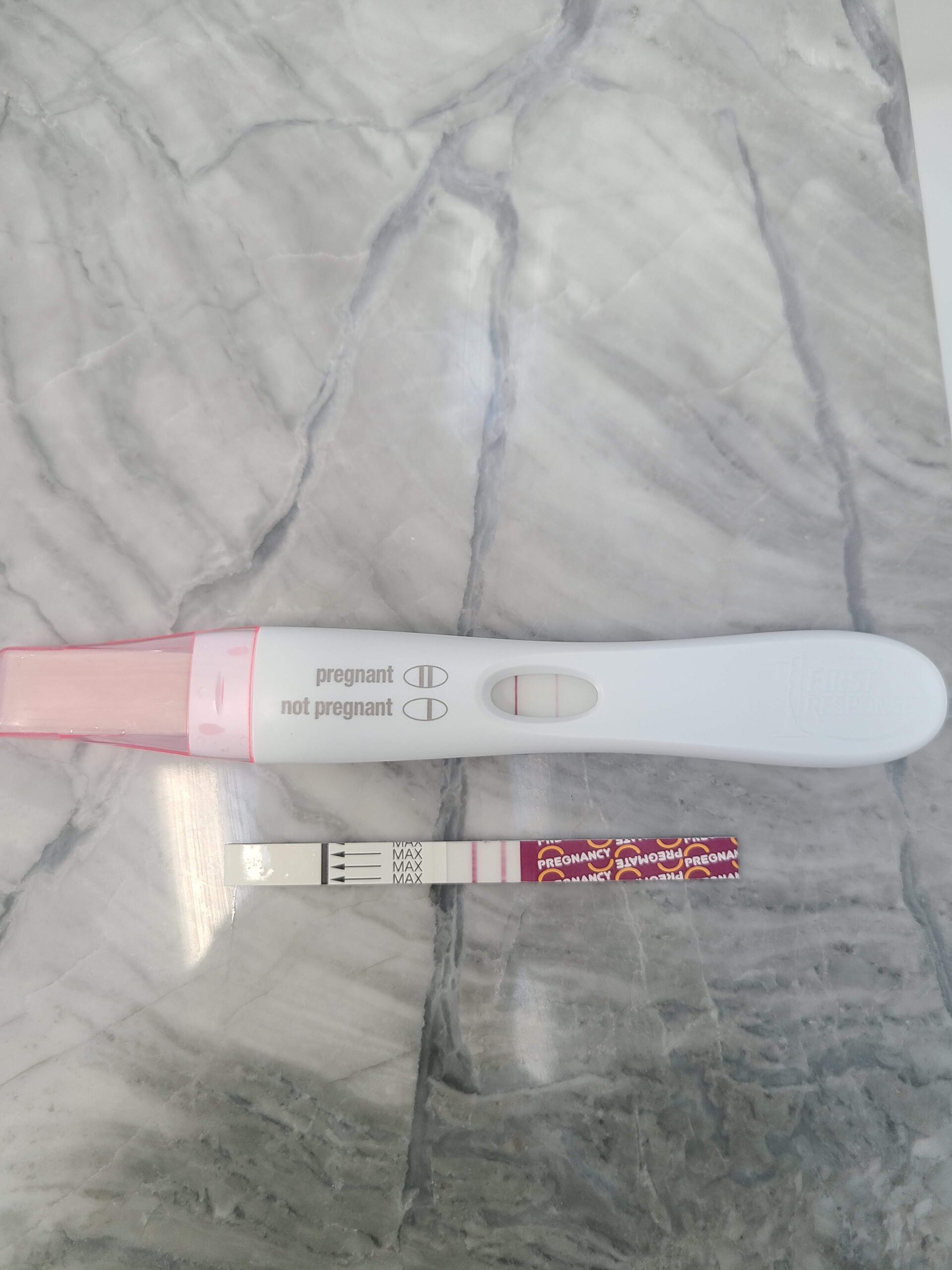
The Two Week Wait is exactly what it sounds like. There is a two week period between the day of the transfer and the day of your first b-hcg blood test. Many, including myself, find this a very very stressful time, but I just tried to stay as busy as possible. I was already relatively busy at work, which was good to keep my mind occupied. During this time, I started taking estrogen pills and we administered intramuscular progesterone shots nightly. Both of these hormones help to provide the right environment for an embryo to hopefully implant. After our two week wait was up, I went in for an early morning blood test and then the worst wait of all started. Eric and I had to wait almost the whole day to get our results back. It wasn’t until almost 4pm that we got the good news…”Congratulations, you’re pregnant”! We couldn’t believe it and we immediately video chatted with our family to tell them the good news. Even though it’s not customary to announce a pregnancy so soon, our entire family was aware that we were going through IVF, so they were waiting for our results as anxiously as we were!
One other thing I wanted to mention is that I did have a minor side effect. I think it was related both to all of the hormonal changes and to stress and anxiety, but I had some shortness of breath during a portion of the two week wait. I immediately called the doctor and they brought me in to do some routine tests, including checking my blood pressure and heart rate. I was told to drink fluids that restore electrolytes, like gatorade. Eventually, the breathlessness subsided but if you have any side effects, no matter how small, definitely consult with your doctor immediately!
WHAT HAPPENS NEXT
From there, we stayed with our fertility clinic for a few more weeks before transitioning to a general obstetrician. During that time, my doctor continued to monitor my b-hcg, progesterone and estrogen levels via blood tests. Once my b-hcg reached a certain level, they transitioned their monitoring to ultrasounds. The first ultrasound was done to confirm that the pregnancy was in my uterus rather than in the tube. From there, it was just typical ultrasound monitoring to confirm fetal growth, monitor the heartbeat (we saw a heartbeat at 6 weeks and heard it at 7 weeks) and we continued weekly blood tests to monitor my progesterone and estrogen levels. I stayed on those two medications for about 10 weeks and stopped taking them right around the time that I transitioned from the IVF clinic over to an OB.
I go into more detail about our loss story in this blog post. I hope this post is helpful for anyone else going through a fertility or IVF journey.









No Comments